
A Comprehensive Guide on Brain Tumours Treatment in India
15 Jun, 2024
Dealing with a brain tumour diagnosis can be overwhelming. Understanding treatment options and choosing the right provider are crucial steps towards recovery. India has become a leading destination for brain tumour treatment, offering advanced technology, skilled professionals, and affordable care. Brain tumours pose significant health risks and require immediate, comprehensive treatment. Finding effective treatments, experienced doctors, and affordable care can be challenging. The complexity of brain tumour treatment adds stress for patients and families. Navigating various treatment options and choosing the best providers can be daunting. This guide provides a detailed overview of brain tumour treatments in India, including procedures, top doctors, renowned hospitals, treatment costs, success rates, associated risks, and post-treatment care. It offers valuable insights to help patients and families make informed decisions and approach treatment with confidence.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Brain Tumours Procedures
Brain tumours can be either benign (non-cancerous) or malignant (cancerous), and their treatment varies accordingly. The primary goal of brain tumour treatment is to remove or destroy the tumour while preserving as much normal brain function as possible. Here are the primary procedures used in brain tumour treatment:
Surgical Procedures for Brain Tumours
1. Craniotomy
A craniotomy is a surgical procedure that involves removing a section of the skull (cranium) to access the brain and treat the tumour. This procedure is performed under general anaesthesia and involves several key steps:
Incision: A neurosurgeon makes an incision in the scalp, usually behind the hairline, to expose the area of the skull where the craniotomy will be performed.
Bone Flap Removal: Using specialized tools like a drill or a saw, the surgeon carefully creates a bone flap in the skull. The size and shape of the bone flap depend on the location and size of the tumour.
Brain Access: Once the bone flap is removed, the dura mater (the tough membrane covering the brain) is opened, allowing access to the brain tissue and the tumour.
Most popular procedures in India
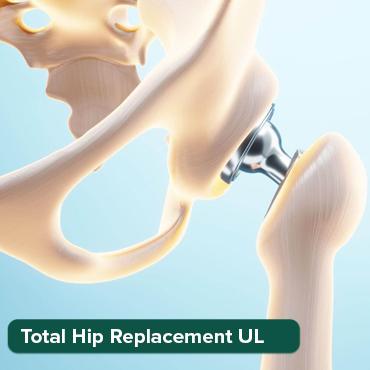
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
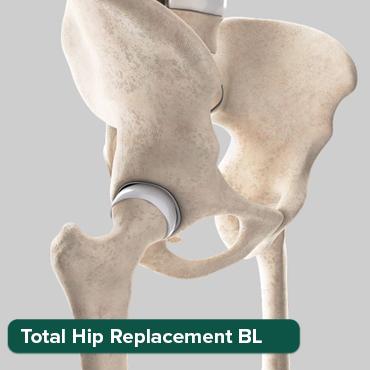
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

Liver Transplant Sur
Upto 80% off
90% Rated
Satisfactory

Tumor Removal: The neurosurgeon then carefully removes as much of the tumor as possible, while aiming to preserve nearby healthy brain tissue and critical structures such as blood vessels and nerves.
Closure: After the tumour removal, the bone flap is replaced and secured with small plates, screws, or wires. The incision in the scalp is closed with stitches or staples.
2. Minimally Invasive Techniques
In recent years, advancements in technology have led to the development of minimally invasive techniques for brain tumour surgery. These approaches aim to reduce trauma to the brain and improve recovery times. Some common minimally invasive techniques include:
Endoscopic Surgery: This involves using a small, flexible tube with a camera (endoscope) and specialized surgical tools to access and remove tumours through small incisions in the scalp or nose. Endoscopic procedures are particularly useful for tumours located in deep or difficult-to-reach areas of the brain.
Stereotactic Biopsy: A stereotactic biopsy is a minimally invasive procedure used to obtain a sample of the tumour tissue for diagnosis. It involves using 3D imaging techniques (such as MRI or CT scans) to precisely guide a biopsy needle to the tumour location.
3. Awake Craniotomy
In some cases, especially when the tumour is located near critical areas of the brain that control functions like speech or movement, an awake craniotomy may be performed. This procedure allows the surgeon to monitor brain function in real time and make adjustments during the surgery to minimize damage to vital areas.
Mapping: Before the tumour removal begins, the patient may be awake and asked to perform tasks such as counting, speaking, or moving specific body parts. This helps the surgeon map out and identify critical areas of the brain that need to be preserved.
Monitoring: During the surgery, electrodes may be placed on the brain's surface to monitor electrical activity and ensure that important functions are not compromised.
4. Robot-Assisted Surgery
Robotic systems can assist neurosurgeons in performing precise movements during brain tumour surgery. These systems use computer-guided technology to enhance the surgeon's accuracy and control, particularly in delicate procedures where precision is crucial.
- Benefits: Robot-assisted surgery can potentially reduce recovery times, minimize trauma to surrounding brain tissue, and improve surgical outcomes.
Post-Surgical Care and Follow-Up
After brain tumour surgery, patients typically require close monitoring and may undergo additional treatments such as:
Radiation Therapy: Used to target any remaining tumour cells that could not be removed surgically.
Chemotherapy: Administered orally or intravenously to kill cancer cells or inhibit their growth.
Rehabilitation: Physical therapy, speech therapy, and occupational therapy may be necessary to help patients regain function and adapt to any changes caused by the surgery.
Follow-Up Imaging: Regular MRI or CT scans are performed to monitor for tumour recurrence and assess the effectiveness of treatment.
In conclusion, surgical treatment of brain tumours involves a range of techniques tailored to the tumour's location, size, and the patient's overall health. Advances in surgical technology continue to improve outcomes and reduce the impact of surgery on patients' quality of life.
2. Radiation Therapy
Radiation therapy is a crucial treatment option for brain tumours, employing high-energy radiation to target and destroy cancer cells or shrink tumours. Here's a detailed explanation of how radiation therapy works, including specific techniques like stereotactic radiosurgery:
1. Principles of Radiation Therapy
Radiation therapy works by damaging the DNA inside cancer cells, preventing them from growing and dividing. This can lead to the death of cancer cells or inhibit their ability to multiply. It is often used in conjunction with surgery and/or chemotherapy to treat brain tumours.
2. Types of Radiation Therapy
External Beam Radiation Therapy (EBRT): This is the most common form of radiation therapy for brain tumours. It involves directing high-energy beams from outside the body (external beam) towards the tumour site. The radiation is carefully shaped and aimed to maximize its impact on the tumour while minimizing exposure to surrounding healthy tissue.
Stereotactic Radiosurgery (SRS): Despite its name, SRS is not surgery in the traditional sense but a highly precise form of radiation therapy. It delivers a concentrated dose of radiation to a small, well-defined target area, such as a brain tumour, in a single session or a few sessions. This approach is particularly effective for small tumours or tumours located in critical or hard-to-reach areas of the brain.
Gamma Knife: Gamma Knife radiosurgery uses multiple beams of gamma radiation to focus precisely on the tumour while sparing healthy brain tissue. It is non-invasive and does not require surgical incisions, making it suitable for certain types of brain tumours.
CyberKnife: CyberKnife is another form of stereotactic radiosurgery that uses a robotic arm to deliver highly precise beams of radiation from multiple angles. It continuously adjusts the radiation beams to track the tumour's movement, such as with breathing, ensuring accurate targeting.
3. Procedure
Treatment Planning: Before radiation therapy begins, the medical team performs imaging tests such as MRI or CT scans to precisely locate the tumour and determine the optimal radiation dose and angles.
Radiation Delivery: During treatment sessions, the patient lies on a treatment table while the radiation machine delivers the prescribed dose of radiation. The sessions are typically short, ranging from a few minutes to an hour, depending on the type of radiation therapy and the complexity of the treatment plan.
Monitoring and Follow-Up: Patients are closely monitored during and after radiation therapy to assess treatment response and manage any side effects. Follow-up imaging scans are performed regularly to monitor tumour size and response to treatment.
4. Side Effects
Radiation therapy can cause side effects, which vary depending on the dose and location of treatment. Common side effects may include fatigue, headaches, hair loss (in the treatment area), skin changes, and temporary swelling or irritation of brain tissue. The medical team takes steps to minimize these effects and support patients throughout their treatment.
5. Advantages
Precision: Techniques like stereotactic radiosurgery allow for highly precise targeting of tumours, minimizing damage to surrounding healthy brain tissue.
Non-Invasive: Many radiation therapy procedures are non-invasive and do not require surgical incisions, reducing recovery times and risks associated with traditional surgery.
Effective: Radiation therapy is effective in controlling tumour growth and improving symptoms, often used in combination with other treatments for optimal results.
In conclusion, radiation therapy, including advanced techniques like stereotactic radiosurgery, plays a critical role in the comprehensive treatment of brain tumours. It offers patients a targeted, effective treatment option with minimal impact on their overall quality of life.
3. Chemotherapy
Chemotherapy is a systemic treatment that uses drugs to destroy cancer cells or inhibit their growth throughout the body. When it comes to brain tumors, chemotherapy can be administered in several ways, depending on the type of tumour, its location, and the overall treatment plan. Here’s a detailed look at how chemotherapy is used for brain tumours:
1. Systemic Chemotherapy
Administration: Chemotherapy drugs can be given orally (in pill form) or intravenously (IV), allowing them to enter the bloodstream and reach cancer cells throughout the body, including those in the brain.
Mechanism of Action: These drugs work by targeting rapidly dividing cells, which include cancer cells. They interfere with the cancer cell's ability to grow and divide, ultimately causing cell death.
Indications: Systemic chemotherapy is often used for brain tumours that have spread from other parts of the body (metastatic tumours) or for certain types of primary brain tumours that are responsive to chemotherapy.
Combination Therapy: Chemotherapy is sometimes used in combination with radiation therapy or surgery to maximize treatment effectiveness.
2. Intrathecal Chemotherapy
Administration: In cases where brain tumors involve the cerebrospinal fluid (CSF) or have spread to the lining of the brain (meninges), chemotherapy drugs can be administered directly into the CSF. This is known as intrathecal chemotherapy.
Procedure: Intrathecal chemotherapy involves injecting drugs into the spinal canal through a needle inserted into the lower part of the spine (lumbar puncture) or through an Ommaya reservoir, a device implanted under the scalp that allows direct access to the CSF.
Purpose: Direct delivery into the CSF allows for higher concentrations of chemotherapy drugs in the central nervous system, targeting cancer cells in the brain and spinal cord.
3. Common Chemotherapy Drugs
Temozolomide: This is one of the most commonly used chemotherapy drugs for treating certain types of brain tumours, such as glioblastoma multiforme (GBM). It is typically administered orally.
Methotrexate: Methotrexate is used in both systemic and intrathecal chemotherapy for brain tumours that involve the CSF or meninges.
Cisplatin, Carboplatin, and others: These drugs may also be used depending on the specific type of brain tumour and its responsiveness to chemotherapy.
4. Side Effects
General Side Effects: Chemotherapy can cause a range of side effects, including fatigue, nausea, vomiting, hair loss, and increased susceptibility to infections. These side effects can vary depending on the type and dose of chemotherapy drugs used.
Neurological Side Effects: Some chemotherapy drugs can cause neurological side effects, such as peripheral neuropathy (nerve damage), cognitive changes, or mood swings.
5. Monitoring and Follow-Up
Response Assessment: Patients undergoing chemotherapy for brain tumours are closely monitored with regular imaging scans (MRI or CT) to assess tumour response to treatment.
Supportive Care: Supportive therapies such as anti-nausea medications, pain management, and nutritional support are often provided to manage side effects and improve quality of life during treatment.
In summary, chemotherapy is an essential component of treatment for many types of brain tumours. Its effectiveness depends on factors such as tumour type, stage, and the patient's overall health. Combined with surgery, radiation therapy, and other treatment modalities, chemotherapy plays a crucial role in improving outcomes and prolonging survival for patients with brain tumours.
4. Targeted Therapy
Targeted therapy is a specialized treatment approach that focuses on targeting specific abnormalities or molecular characteristics present within cancer cells. Unlike traditional chemotherapy, which affects both cancerous and healthy cells, targeted therapy aims to interfere with the specific molecules or pathways that promote tumour growth and survival. Here’s a detailed overview of targeted therapy for cancer:
1. Mechanisms of Targeted Therapy
Specific Targeting: Targeted therapy drugs are designed to selectively target proteins or genetic mutations that are found predominantly within cancer cells or tumour-associated cells.
Interference with Tumor Growth: By blocking specific molecules or pathways essential for cancer cell proliferation, targeted therapy aims to inhibit tumour growth and promote cancer cell death.
Types of Targets: Targets of targeted therapy may include:
Receptor Tyrosine Kinases: Proteins on the surface of cancer cells that promote cell growth and division.
Angiogenesis Inhibitors: Drugs that target the formation of new blood vessels that tumours need to grow.
Signal Transduction Pathways: Intracellular pathways that regulate cell survival and proliferation.
Gene Mutations: Specific mutations in genes (e.g., EGFR, BRAF) that drive cancer growth.
2. Benefits of Targeted Therapy
Precision: Targeted therapy drugs are designed to specifically attack cancer cells while minimizing damage to healthy cells, reducing potential side effects compared to traditional chemotherapy.
Improved Effectiveness: In some cases, targeted therapy can be more effective than conventional treatments, particularly for cancers with specific genetic mutations or biomarkers.
Combination Therapies: Targeted therapies are often used in combination with other treatments such as chemotherapy, radiation therapy, or immunotherapy to enhance treatment outcomes.
3. Examples of Targeted Therapy Drugs
Imatinib (Gleevec): Targets a specific fusion protein (BCR-ABL) found in chronic myelogenous leukaemia (CML) and certain types of gastrointestinal stromal tumours (GISTs).
Trastuzumab (Herceptin): Targets HER2/neu receptors overexpressed in some breast cancers and stomach cancers.
Erlotinib (Tarceva) and Gefitinib (Iressa): Target EGFR mutations found in non-small cell lung cancer (NSCLC).
BRAF Inhibitors (e.g., Vemurafenib): Target BRAF gene mutations present in melanoma and other cancers.
4. Administration and Side Effects
Oral Medications: Many targeted therapy drugs are administered orally, and taken as pills or tablets, making them convenient for patients undergoing long-term treatment.
Side Effects: While generally well-tolerated, targeted therapy can still cause side effects such as skin rash, diarrhoea, liver toxicity, hypertension, and in some cases, cardiovascular complications. The side effects vary depending on the specific drug and individual patient factors.
5. Monitoring and Response Evaluation
Monitoring: Regular monitoring through imaging tests and blood tests helps assess tumour response and detect any potential side effects early.
Response Evaluation: Response to targeted therapy is evaluated based on tumour shrinkage, stabilization, or progression, guiding adjustments in treatment as needed.
In summary, targeted therapy represents a significant advancement in cancer treatment, offering personalized and effective options for patients with specific molecular characteristics in their tumours. As research continues, the development of new targeted therapies holds promise for improving outcomes and quality of life for individuals facing cancer.
5. Immunotherapy
Immunotherapy is a revolutionary treatment approach that harnesses the body's own immune system to combat cancer. Unlike traditional treatments like chemotherapy, which directly target cancer cells, immunotherapy works by enhancing the immune system's ability to recognize and destroy cancer cells. Here’s an in-depth look at how immunotherapy is used in cancer treatment, including its various forms and mechanisms:
1. Monoclonal Antibodies
Mechanism: Monoclonal antibodies are laboratory-made proteins that can specifically bind to certain targets on cancer cells. They can act in different ways:
- Direct Action: By attaching to cancer cells, antibodies can interfere with their growth and survival mechanisms.
- Immune System Activation: Antibodies can also flag cancer cells for destruction by immune cells like T cells or macrophages.
Examples: Drugs like Rituximab (used in lymphomas), Trastuzumab (used in breast cancer), and Pembrolizumab (Keytruda) are examples of monoclonal antibodies used in cancer treatment.
2. Checkpoint Inhibitors
Mechanism: Checkpoint inhibitors block inhibitory pathways in the immune system that cancer cells exploit to evade detection and attack by the immune system. By releasing these brakes, checkpoint inhibitors allow the immune system to mount a more effective response against cancer cells.
Examples: Drugs such as Pembrolizumab (Keytruda), Nivolumab (Opdivo), and Ipilimumab (Yervoy) target checkpoints like PD-1, PD-L1, and CTLA-4.
3. Cancer Vaccines
Mechanism: Cancer vaccines are designed to stimulate the immune system to recognize and attack cancer cells. They may contain tumour-specific antigens or genetic material from cancer cells to provoke an immune response against cancer.
Types: There are different types of cancer vaccines:
- Preventive Vaccines: Aimed at preventing certain cancers caused by infectious agents (e.g., HPV vaccines for cervical cancer).
- Therapeutic Vaccines: Used to treat existing cancer by boosting the immune response against tumour cells.
4. Adoptive Cell Therapy
Mechanism: Adoptive cell therapy involves harvesting a patient's own immune cells (such as T cells), modifying them in the lab to better recognize and attack cancer cells, and then reintroducing them into the patient.
CAR T-cell Therapy: Chimeric Antigen Receptor (CAR) T-cell therapy is a type of adoptive cell therapy where T cells are engineered to express specific receptors (CARs) that recognize and bind to proteins on cancer cells, enhancing their ability to target and destroy cancer cells.
5. Uses and Effectiveness
Indications: Immunotherapy is used in various cancers, including melanoma, lung cancer, bladder cancer, kidney cancer, and certain types of lymphomas and leukaemias.
Effectiveness: While not effective for all patients or all types of cancer, immunotherapy has shown remarkable results in some cases, leading to durable responses and improved survival rates in subsets of patients.
6. Side Effects
Immune-Related Adverse Events: Because immunotherapy works by stimulating the immune system, it can lead to immune-related side effects, such as inflammation of the lungs, intestines, liver, or other organs.
Management: Prompt recognition and management of these side effects are crucial for minimizing their impact and allowing patients to continue treatment safely.
Immunotherapy represents a paradigm shift in cancer treatment, offering targeted and potentially long-lasting responses by leveraging the body's immune defences. Ongoing research continues to expand the applications and effectiveness of immunotherapy, paving the way for more personalized and effective cancer treatments in the future.
Top Hospitals for Brain Tumour Treatment in India
India boasts several world-class hospitals equipped with state-of-the-art technology and highly trained medical professionals. These hospitals are known for their comprehensive brain tumour treatment programs:
India is home to some of the finest hospitals known for their expertise in cardiac surgeries, including mitral valve replacement. These hospitals are equipped with state-of-the-art facilities and highly skilled medical professionals. Some of the top hospitals include:
1. Apollo Hospitals, Chennai

Apollo Hospitals on Greams Road in Chennai was established in 1983 by Dr Prathap C Reddy. It was India's first corporate hospital and is acclaimed for pioneering the private healthcare revolution in the country. Over the years, Apollo Hospitals has risen to a position of leadership, emerging as Asia's foremost integrated healthcare services provider.
Location
- Address: 21 Greams Lane, Off Greams Road, Thousand Lights, Chennai, Tamil Nadu 600006, India
- City: Chennai
- Country: India
Hospital Features
- Established Year: 1983
- Treatment Availability: International
- Hospital Category: Medical
- Status: Active
- Visibility on Website: Yes
About Apollo Hospitals
Apollo Hospitals has a robust presence across the healthcare ecosystem, including hospitals, pharmacies, primary care, and diagnostic clinics. The Group also has telemedicine units across 10 countries, health insurance services, global projects consultancy, medical colleges, Med-varsity for e-learning, colleges of nursing, and hospital management.
Team and Specialties
- Cardiology and Cardiothoracic Surgery: Apollo Hospitals hosts one of the largest cardiovascular groups globally, with around 14 world-class institutes, over 400 cardiologists & cardiac surgeons, and 200 heart stations.
- Robotic Spinal Surgery: Among the few centres in Asia to perform this advanced procedure, Apollo is at the forefront of spinal disorder management.
- Cancer Care: A 300-bedded, NABH-accredited hospital providing advanced technology in diagnosis and radiation, supported by an oncology team of renowned specialists and well-trained medical and paramedical professionals.
- Gastroenterology: Offers the latest endoscopic procedures for gastrointestinal bleeding, cancers, foreign body removal, etc.
- Transplant Institutes: The Apollo Transplant Institutes (ATI) is one of the largest, most comprehensive, and busiest solid transplant programs globally.
- Liver Surgery: Equipped with a 320-slice CT scanner, a state-of-the-art Liver Intensive Care Unit & Operation Theatre, and various surgical tools to enable safe & bloodless liver surgery.
- Neurosurgery: Recognized as a leader in acute neurosurgery, Apollo Hospitals, Chennai, is among the top hospitals specializing in neuro care worldwide.
Infrastructure
With the experience of over one million health checks, Apollo Hospitals has emerged as a key player in the corporate healthcare sector. Over 500 leading corporates, across all industry segments, have tied up with Apollo Hospitals, providing their employees ready access to sophisticated medical facilities at over 64 locations in India. The corporate services initiative of Apollo Hospitals, Chennai, aims to provide world-standard healthcare within the reach of every individual.
2. Fortis Memorial Research Institute (FMRI), Gurugram

Fortis Memorial Research Institute (FMRI) in Gurgaon is a premier multi-super specialty, quaternary care hospital. Known for its international faculty and reputed clinicians, including super-sub-specialists and speciality nurses, FMRI is supported by cutting-edge technology. The hospital aims to be the 'Mecca of Healthcare' for the Asia Pacific region and beyond.
Location
- Address: Sector - 44, Opposite HUDA City Centre, Gurgaon, Haryana - 122002, India
- City: Gurgaon
- Country: India
Hospital Features
- Established Year: 2001
- Number of Beds: 1000
- Number of ICU Beds: 81
- Operation Theaters: 15
- Hospital Category: Medical
- Treatment Availability: International
- Status: Active
- Visibility on Website: Yes
Specialties
FMRI excels in several medical specialities, including:
- Neurosciences
- Oncology
- Renal Sciences
- Orthopedics
- Cardiac Sciences
- Obstetrics and Gynecology
These specialities leverage advanced technology and top clinicians to deliver exceptional healthcare services.
Team and Expertise
- International Recognition: FMRI has been ranked No.2 of the 30 most technologically advanced hospitals in the world by ‘topmastersinhealthcare.com,’ surpassing many other outstanding medical institutions globally.
- Patient Care: Fortis hospitals treat over 3.5 lakh patients annually, relying on reputed clinicians, state-of-the-art infrastructure, and world-class technology such as the Da Vinci robot, ensuring patients go home healthy.
- Innovative Initiatives: FMRI's initiatives range from customized preventive health checks to quaternary care provided by super-specialized clinicians conducting rare and complex surgeries.
About Fortis Healthcare
FMRI is a flagship hospital of Fortis Healthcare, one of the top healthcare providers in India. Fortis Healthcare is known for its commitment to quality healthcare and patient safety, making FMRI one of the most sought-after medical destinations in the region.
3. Indraprastha Apollo Hospital, New Delhi

- Address: Indraprastha Apollo Hospitals, Sarita Vihar, Delhi-Mathura Road, New Delhi - 110076, India
- Country: India
- Treatment Availability: Both (Domestic & International)
- Hospital Category: Medical
About Hospital:
- Indraprastha Apollo Hospitals, New Delhi, is a multi-speciality tertiary acute care hospital with 710 beds, making it one of the most sought-after destinations in Asia for healthcare.
- It is a state-of-the-art modern facility in the heart of the capital, spread over 15 acres with a built-up area of over 600,000 square feet.
- This flagship hospital of the Apollo Hospitals Group epitomizes the clinical excellence that the Apollo Group stands for, aiming for the best clinical outcomes for patients.
- The hospital achieves the best clinical outcomes for the most complex diseases with the best staff supported by the latest technology and standardized processes.
- Indraprastha Apollo Hospitals engages the best consultants through a rigorous credentialing and privileging process, supported by top healthcare staff.
- Regular training programs, conferences, and continuing medical education programs keep the staff abreast of the latest developments in their fields.
- The hospital is equipped with the latest and best-in-class medical technologies such as PET-MR, PET-CT, Da Vinci Robotic Surgery System, Brainlab Navigation System, Portable CT Scanner, NovalisTx, Tilting MRI, Cobalt-based HDR Brachytherapy, DSA Lab, Hyperbaric Chamber, Fibroscan, Endosonography, 3 Tesla MRI, and 128 Slice CT scanner to provide world-class care.
- Indraprastha Apollo Hospitals was the first hospital in India to be JCI accredited in 2005 and was the first to be reaccredited in 2008 and 2011. It also has NABL-accredited clinical laboratories and a state-of-the-art blood bank.
Team and Speciality:
- The hospital has a team of the best consultants supported by top healthcare staff, engaging in regular training and continuous education.
Infrastructure:
- Established in 1996
- Number of Beds: 1000
- State-of-the-art facilities with the latest medical technologies.
Cost of Bile Duct Cancer Treatment in India (USD)
The cost of bile duct cancer treatment in India varies based on the type of treatment and the hospital. On average:
- Surgery: $5,000 - $15,000
- Radiation Therapy: $3,000 - $7,000
- Chemotherapy: $1,000 - $5,000 per cycle
- Targeted Therapy: $2,000 - $10,000 per month
These hospitals and doctors are recognized for their expertise and commitment to providing high-quality care, making India a preferred destination for brain tumour treatment.
Brain Tumor Treatment Cost in India
The cost of brain tumour treatment in India varies depending on several factors:
- Type of surgery: Minimally invasive surgery generally costs less than craniotomy (opening the skull).
- Tumor location and complexity: More complex surgeries or those on critical areas of the brain may be more expensive.
- Hospital facilities and surgeon's experience: Renowned surgeons and well-equipped hospitals tend to have higher costs.
- Length of hospital stay and post-surgical care: This can vary depending on the complexity of the surgery and your recovery.
Here's a general range for brain tumour surgery costs in India:
- Minimum: ₹1,50,000 (approx. USD $1,800)
- Maximum: ₹5,00,000 (approx. USD $6,000)
Additional Costs:
- Radiation therapy and chemotherapy can add to the overall treatment cost.
- Medication and follow-up consultations will also incur additional expenses.
Brain Tumor Treatment Success Rate in India
Success rates for brain tumour treatment in India are generally considered good. However, they depend on various factors:
- Type and grade of tumour: Benign tumours have a higher success rate than malignant ones.
- Tumor location and size: Early detection and tumours in less critical areas offer a better prognosis.
- Patient's overall health: Age, pre-existing conditions, and response to treatment can influence success rates.
While specific success rates for hospitals might be difficult to find, here's what you can expect:
- Reported Success Rates: Studies suggest an overall success rate exceeding 90% for certain brain tumour surgeries in India.
- Individualized Rates: Consult with your doctor for a personalized success rate estimate based on your specific condition.
Here are some resources for further exploration:
- Hospital Websites: Many hospitals in India advertise their experience with brain tumour procedures on their websites.
- Medical Associations: Indian medical associations of neurosurgery might publish data on brain tumour treatment outcomes.
Remember, this information is for general knowledge. It's crucial to consult with a qualified medical professional for personalized advice on brain tumour treatment options and success rates in your specific case.
How can HealthTrip assist with your treatment?
If you're seeking Brain Tumours Treatment in India, let HealthTrip be your compass. We support you throughout your medical journey with the following:
- Access to top doctors in 38+ countries and the largest health travel platform.
- Partnerships with 1500+ hospitals, including Fortis, Medanta, and more.
- Treatments in neuro, cardiac care, transplants, aesthetics, and wellness.
- Post-treatment care and assistance.
- Teleconsultations with leading doctors at $1/minute.
- Over 61K patients served.
- Access Top treatments and packages, such as Angiograms and many more.
- Gain insights from genuine patient experiences and testimonials.
- Stay updated with our medical blog.
- 24/7 unwavering support, from hospital formalities to travel arrangements or emergencies.
Risks Associated with Brain Tumour Treatment
While brain tumour treatments can be highly effective, they also come with potential risks and side effects, including:
- Infection: Post-surgical infections are a risk.
- Bleeding: Risk of bleeding during or after surgery.
- Neurological Damage: Potential damage to brain tissue, affecting functions like speech, movement, or memory.
- Fatigue: Common side effect of radiation and chemotherapy.
- Nausea and Vomiting: Often associated with chemotherapy.
Post-Treatment Care and Recovery
Post-treatment care is crucial for recovery and includes:
- Regular Follow-ups: Regular monitoring through MRI or CT scans.
- Rehabilitation: Physical therapy, occupational therapy, and speech therapy to regain lost functions.
- Medication: Medications to manage pain and prevent infections.
- Supportive Care: Psychological support and counselling for patients and families.
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!








