
Understanding ulcerative colitis: A comprehensive guide
11 Aug, 2023
 Healthtrip Team
Healthtrip TeamUnderstanding ulcerative colitis: A comprehensive guide
Ulcerative colitis (UC) is a chronic inflammatory bowel disease affecting the inner lining of the large intestine and rectum. Beyond its physical symptoms, UC also poses emotional and psychological challenges for those diagnosed. This guide provides a comprehensive look into UC, from its causes to the latest in research and treatment. Join us as we delve into understanding this complex condition.
Ulcerative colitis (UC)
Hey there! Let's dive into understanding ulcerative colitis (UC). At its core, UC is a chronic inflammatory bowel disease (IBD) that specifically targets the innermost lining of your large intestine (which we often call the colon) and the rectum. Imagine the inner walls of these parts of your digestive system getting inflamed and developing tiny sores or ulcers. That's essentially what's happening in UC.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Now, when we talk about how common this condition is or who it affects, we're diving into the realm of epidemiology. Globally, UC has been on the radar for quite some time, and its prevalence (meaning the total number of cases at a given time) and incidence (which refers to the number of new cases over a specific period) vary depending on the region. For instance, in Western countries, the prevalence can be as high as 250 cases per 100,000 people. The incidence, on the other hand, might range from 10 to 20 new cases per 100,000 people annually.
Demographically speaking, UC doesn't play favorites. It can affect anyone, regardless of age. However, there are two age groups where we see a bit of a spike: one in young adults (between 15 and 30 years old) and another smaller peak in those over 60. Both men and women can get UC, but the distribution is pretty even between the genders.
So, in a nutshell, UC is this chronic condition affecting the colon and rectum, and while it's more common in some parts of the world than others, it's something that medical professionals across the globe are familiar with and actively manage.
2. Etiology and Pathogenesis
Alright, let's delve into the "why" and "how" of ulcerative colitis (UC). Essentially, why does it happen, and how does it develop in the body?
1. Genetic predisposition:
Think of our genes as a blueprint for how our body operates. Sometimes, certain patterns in this blueprint can make a person more susceptible to developing specific conditions. In the case of UC, there's evidence that if someone in your family has had it, you might be at a higher risk. While no single "UC gene" has been identified, multiple genes are believed to play a role. So, if UC is a common topic at family gatherings, it might not just be a coincidence.
2. Immune system response:
Our immune system is like our body's security team, always on the lookout for harmful invaders like viruses or bacteria. But sometimes, this system can get a bit overzealous. In UC, there's a theory that the immune system mistakenly targets the cells of the colon's lining, thinking they're foreign invaders. This misguided attack leads to inflammation and the symptoms we associate with UC. Some believe this immune response might initially be triggered by a virus or bacterium, but the body continues to attack even after the actual threat is gone.
Most popular procedures in India
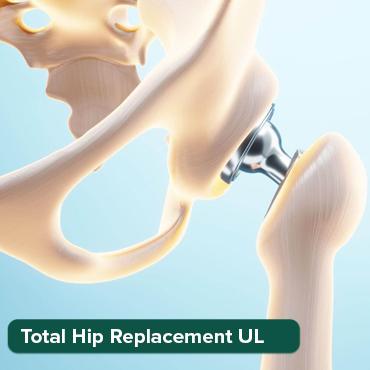
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
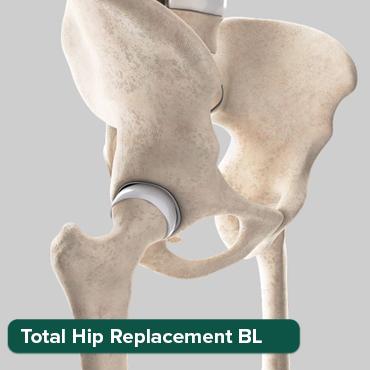
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

Liver Transplant Sur
Upto 80% off
90% Rated
Satisfactory

3. Environmental factors:
Where you live, what you eat, and how you live your life can all play a role in UC. For instance, UC is more common in urban areas and developed countries. Factors like a high-fat diet, high sugar intake, or even frequent use of nonsteroidal anti-inflammatory drugs (like ibuprofen) have been linked to UC. It's like a puzzle, and while we don't have all the pieces yet, we know that environment is a significant part of the picture.
4. Gut microbiota:
Our gut is like a bustling city, home to trillions of bacteria, fungi, and other microorganisms. This community, known as the gut microbiota, plays a crucial role in our health. In people with UC, the balance of this community seems to be off. Some harmful bacteria might be more prevalent, while some beneficial ones might be in short supply. This imbalance, known as dysbiosis, could contribute to the inflammation and other symptoms of UC.
In essence, UC is a complex condition with multiple factors at play. It's like a jigsaw puzzle where genetics, immune responses, environmental factors, and our very own gut residents all interlock to create the bigger picture.
Clinical Presentation
Alright, let's chat about how ulcerative colitis (UC) typically presents itself. When someone has UC, their body gives off certain signs and symptoms, which are like clues that help doctors identify what's going on.
Symptoms:
When UC is active, here's what might be happening:
- Diarrhea (often with blood): This is one of the hallmark symptoms. The inflammation in the colon makes it hard for it to absorb water, leading to loose stools. The ulcers can also bleed, which is why someone might notice blood in their stool.
- Abdominal pain and cramping: Imagine the inner lining of your colon being inflamed and irritated. This can lead to a feeling of discomfort or even sharp pains in the belly, especially around the lower left side.
- Urgency to defecate: With UC, the rectum becomes inflamed, making someone feel like they need to go to the bathroom urgently, even if they've just been.
- Weight loss: This isn't about trying to shed a few pounds. The inflammation can make it hard for the body to absorb nutrients, leading to unintentional weight loss. Plus, the abdominal pain might make someone less keen on eating.
- Fatigue: Feeling tired or drained is common. This can be due to the body fighting inflammation, loss of nutrients, or even anemia from blood loss.
Extraintestinal manifestations:
Now, UC doesn't just stop at the gut. Sometimes, other parts of the body chime in with their own set of issues:
- Joint pain: This is also known as arthralgia. Some people with UC might feel pain or even swelling in their joints, especially in the knees, ankles, wrists, and elbows.
- Skin lesions: UC can sometimes be accompanied by skin issues like erythema nodosum (red, tender lumps usually on the shins) or pyoderma gangrenosum (painful ulcers on the skin).
- Eye inflammation: Conditions like uveitis (inflammation of the middle layer of the eye) or episcleritis (inflammation of the white part of the eye) can occur. This might make the eyes red, painful, or sensitive to light.
- Liver disorders: While less common, UC can be linked to conditions like primary sclerosing cholangitis, where the bile ducts in the liver become inflamed and scarred.
In a nutshell, UC is like an iceberg. While the gut symptoms are the most visible part, there's a lot more going on beneath the surface that can affect various parts of the body.
Diagnosis
Alright, so someone's showing signs of ulcerative colitis (UC). How do we confirm it? Diagnosing UC is a bit like detective work, piecing together various clues to get a clear picture. Let's walk through the process.
History and physical examination:
First and foremost, a doctor will have a chat with the patient. They'll ask about symptoms, their duration, any family history of UC or other gastrointestinal diseases, and other relevant health information. A physical examination will follow, where the doctor might check for abdominal tenderness, listen to bowel sounds, and assess the overall health of the patient.
Laboratory tests:
These are like the basic tools in our diagnostic toolkit.
- Blood tests: These can reveal a lot. For instance, if someone has anemia, it might be due to blood loss from those inflamed ulcers in the colon. Elevated white blood cell counts or other markers can hint at inflammation or infection.
- Stool tests: By analyzing a stool sample, doctors can rule out other causes of gastrointestinal symptoms, like infections or parasites. They can also check for blood in the stool, which might not always be visible to the naked eye.
Endoscopic procedures:
These are more direct ways to peek inside the colon.
- Sigmoidoscopy: This procedure involves inserting a flexible tube with a camera into the rectum to examine the sigmoid colon (the last part of the colon). It gives a close-up view of any inflammation or ulcers.
- Colonoscopy: This is similar to a sigmoidoscopy but allows the doctor to examine the entire colon. It's the gold standard for diagnosing UC. Plus, during a colonoscopy, the doctor can take small tissue samples (biopsies) to examine under a microscope, which can provide more definitive evidence of UC.
Imaging studies:
Sometimes, we need a broader view or a different perspective to understand what's going on.
- X-ray: While not as commonly used for diagnosing UC, an abdominal X-ray can help rule out other conditions or complications like a perforated colon.
- CT scan: This provides a detailed cross-sectional image of the abdomen, which can be useful to assess the extent of inflammation or to spot complications.
- MRI: Magnetic Resonance Imaging offers even more detailed images than a CT scan. It's especially useful for looking at the small intestine or assessing fistulas (abnormal connections between the intestine and other structures).
In essence, diagnosing UC is a comprehensive process. It's about gathering as much information as possible, from both the patient and various tests, to ensure an accurate diagnosis and the best possible care.
Classification
When it comes to ulcerative colitis (UC), not all cases are created equal. The disease can vary in its extent (how much of the colon it affects) and its severity (how intense the symptoms are). To make sense of these variations and to guide treatment, doctors classify UC into different categories. Let's break them down:
Based on extent and severity:
- Ulcerative proctitis:
- Extent: This is the mildest form of UC in terms of extent. It affects only the rectum, which is the last part of the colon before the anus.
- Symptoms: Patients might experience rectal bleeding, rectal pain, and an urgency to defecate. Because of its limited extent, systemic symptoms like fever and fatigue are less common.
- Treatment: Often, a topical treatment (like a suppository or enema) can be effective since the inflammation is so localized.
- Left-sided colitis:
- Extent: As the name suggests, this form affects the left side of the colon, which includes the rectum, sigmoid colon, and sometimes the descending colon.
- Symptoms: Apart from the symptoms seen in ulcerative proctitis, patients might also experience abdominal cramping, weight loss, and some might have loose stools with blood.
- Treatment: Depending on the severity, treatments can range from oral medications to more potent systemic drugs.
- Pancolitis or extensive colitis:
- Extent: This is a more extensive form of UC, affecting the entire colon, from the rectum to the cecum.
- Symptoms: Symptoms can be more severe and might include significant weight loss, abdominal pain, and frequent bouts of diarrhea. Systemic symptoms like fatigue, fever, and night sweats can also be present.
- Treatment: Given the extensive nature, treatment often involves systemic medications, including corticosteroids, immunomodulators, or biologics.
- Acute severe ulcerative colitis:
- Extent: This is a severe, acute flare of UC that can affect any part of the colon but is particularly concerning due to its intensity.
- Symptoms: Patients might experience frequent diarrhea (potentially 10 or more times a day), severe abdominal pain, dehydration, and fever. This condition can be life-threatening and often requires hospitalization.
- Treatment: Immediate intervention is crucial. High-dose intravenous corticosteroids are typically the first line of treatment. If there's no improvement, other treatments like cyclosporine or infliximab might be considered. In some cases, if medications don't help, surgery might be necessary.
By classifying UC into these categories, doctors can tailor treatments to the specific needs of each patient, ensuring they get the most appropriate and effective care.
Prognosis
Understanding the likely course and outcome of ulcerative colitis (UC) can help both patients and doctors make informed decisions about treatment and lifestyle adjustments.
Factors affecting prognosis:
- Extent of the disease: Patients with limited disease (like ulcerative proctitis) generally have a milder course than those with extensive colitis.
- Severity of symptoms: Acute severe ulcerative colitis can be life-threatening and may require more aggressive treatments or even surgery.
- Response to treatment: Patients who respond well to initial treatments often have a better prognosis than those who don't.
- Complications: The presence of complications, such as toxic megacolon or colorectal cancer, can influence the prognosis.
- Age at diagnosis: Earlier onset might be associated with a more severe disease course.
- Extraintestinal manifestations: The presence of symptoms outside the intestine, like joint pain or skin lesions, can indicate a more systemic form of the disease.
Long-term outlook
While UC is a chronic condition with no known cure, many patients can achieve long periods of remission with appropriate treatment. Flares can occur, but with close monitoring and adjustments in treatment, they can be managed. Over time, the risk of colorectal cancer increases, so regular screenings are essential. Some patients, especially those with severe or refractory disease, might require surgery, which can offer a definitive cure but comes with its own set of challenges and adjustments.
Living with Ulcerative Colitis
Living with UC is not just about managing physical symptoms; it encompasses a holistic approach that addresses emotional, psychological, and lifestyle aspects.
Emotional and psychological impact:
- Anxiety and Depression: The unpredictability of flares, concerns about body image, and the chronic nature of UC can lead to anxiety and depression.
- Stress: Stress can be both a result of UC and a potential trigger for flares.
- Self-esteem: Issues like fecal incontinence can impact self-worth and confidence.
Diet and nutrition:
- Individualized approach: There's no one-size-fits-all diet for UC. What works for one person might not work for another.
- Avoiding triggers: Some patients find that specific foods can exacerbate their symptoms.
- Nutritional deficiencies: Due to reduced absorption, patients might need supplements like iron, vitamin B12, or folic acid.
- Hydration: Diarrhea can lead to dehydration, so drinking enough fluids is crucial.
Support groups and counseling:
- Peer support: Connecting with others who have UC can provide emotional support, understanding, and practical advice.
- Professional counseling: Therapists or counselors can help patients cope with the emotional and psychological challenges of UC.
- Education: Understanding the disease can empower patients to take an active role in their care.
In essence, living with UC is a journey that requires a comprehensive approach, addressing not just the physical but also the emotional and psychological aspects of the disease. With the right support and resources, many patients can lead fulfilling lives despite their diagnosis.
Research and future directions
The realm of ulcerative colitis (UC) research is dynamic and ever-evolving. As we strive to understand the disease better, several promising areas are emerging:
- Emerging treatments:
- Biologics: These are drugs that target specific parts of the immune system. Newer biologics are being developed to target different pathways involved in inflammation.
- JAK inhibitors: These are oral medications that block the Janus kinase (JAK) pathways, which play a role in immune responses.
- Stem cell therapy: Research is ongoing to see if stem cells can help repair damaged tissues in the colon.
- Fecal microbiota transplantation (FMT): Introducing healthy donor fecal matter into a patient's gut to restore a balanced microbiome is being explored as a potential treatment.
- Genetic research:
- Genome-wide association studies (GWAS): These studies aim to identify genetic markers associated with UC, which can provide insights into its causes and potential treatments.
- Personalized medicine: By understanding an individual's genetic makeup, treatments can be tailored to offer the best possible outcomes.
- Microbiome studies:
- Gut flora profiling: By understanding the composition of the gut microbiota in UC patients versus healthy individuals, we can gain insights into the role of bacteria in disease progression and remission.
- Probiotic and prebiotic therapies: Research is focusing on introducing or promoting beneficial bacteria to restore gut balance and reduce inflammation.
Ulcerative colitis is a multifaceted condition that intertwines the physical, emotional, and psychological aspects of an individual's life. From its initial presentation to the long-term journey of living with the disease, UC presents challenges that require a holistic approach to care. The landscape of UC research is promising, with emerging treatments and insights that hold the potential to revolutionize how we understand and manage the disease. This outline offers a snapshot of UC, but like any medical topic, the depth and breadth of information available are vast. As we continue to expand our knowledge, the hope is to improve the quality of life for those affected and, ultimately, find a cure.
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!







