Personalized Cancer Treatment Plans in UAE
21 Jul, 2024
 Healthtrip Team
Healthtrip TeamCancer treatment has evolved significantly over the past decade, moving away from a one-size-fits-all approach to more personalized treatment plans. In the UAE, top hospitals are at the forefront of this medical revolution, offering tailored cancer therapies that consider each patient's unique genetic makeup, lifestyle, and specific type of cancer. This blog explores how personalized cancer treatment plans are developed and implemented in leading UAE hospitals, providing patients with hope and improved outcomes.
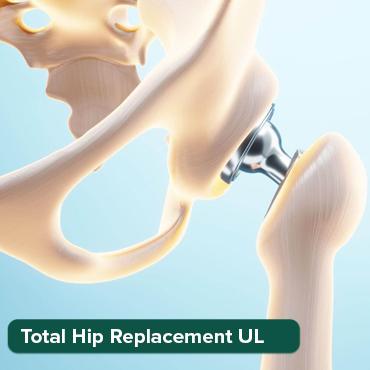
Most popular procedures in India
What is Personalized Cancer Treatment?
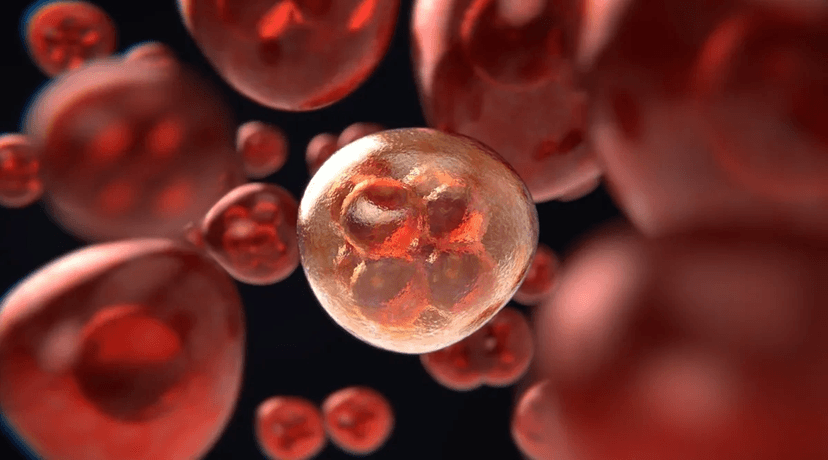
Personalized cancer treatment, also known as precision medicine, involves customizing healthcare tailored to the individual characteristics of each patient. This approach uses genetic, environmental, and lifestyle factors to develop targeted therapies. By understanding the specific mutations and biomarkers present in a patient’s cancer, doctors can design more effective treatment plans that reduce side effects and improve survival rates.
1. Genomic Testing
Genomic testing is a cornerstone of personalized cancer treatment. This approach involves analyzing the genetic material of cancer cells to uncover specific mutations or alterations that drive the growth and spread of cancer. By understanding these genetic changes, doctors can design more effective and targeted treatment plans.
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
Types of Genomic Testing
1. Whole Genome Sequencing (WGS)
Whole Genome Sequencing looks at the entire DNA sequence of an organism’s genome. In the context of cancer care, it offers a complete picture of all the genetic changes that might be affecting the cancer cells. For instance, if someone is diagnosed with lung cancer, WGS might uncover a rare mutation in the EGFR gene (epidermal growth factor receptor). This specific mutation can drive the growth of non-small cell lung cancer (NSCLC). With this knowledge, doctors can prescribe treatments like Erlotinib or Gefitinib that target the mutated EGFR protein, making the treatment more effective.
Whole Exome Sequencing zeroes in on the parts of the DNA that actually code for proteins. Since most cancer-related mutations occur in these areas, WES is often used to spot actionable mutations. Take a patient with breast cancer, for example. If they undergo WES and a mutation in the BRCA1 gene is found, it’s a significant finding. This mutation increases the risk of breast and ovarian cancers. Knowing this, doctors can use treatments like PARP inhibitors, such as Olaparib, which specifically target cancer cells with BRCA1 mutations and can lead to better treatment results.
Targeted gene panels are tests designed to look at specific genes known to be linked to various cancers. They help identify mutations that are relevant to certain types of cancer. For example, if a patient has colon cancer and they’re tested with a targeted gene panel, which includes genes like KRAS, NRAS, and BRAF, it might reveal a mutation in the BRAF gene. This information helps doctors choose targeted treatments like BRAF inhibitors, such as Vemurafenib, which are designed to specifically tackle the mutated BRAF protein and provide a more personalized and effective treatment.
Benefits of Genomic Testing
a. Precision Medicine: Genomic testing helps identify specific genetic mutations in cancer cells, which allows for more precise and targeted treatments. This means patients can avoid the one-size-fits-all approach of traditional treatments that might not work as well for them.
b. Personalized Treatment Plans: Thanks to detailed genetic information, doctors can create treatment plans that are tailored to the unique genetic makeup of the patient’s cancer. This personalization boosts the chances of the treatment being successful.
c. Predictive and Prognostic Insights: Genomic testing can offer clues about how a patient’s cancer might behave and how it could respond to various treatments. This valuable information helps doctors make better decisions about the most effective treatment strategies.
Example in Practice
Take the case of a patient diagnosed with melanoma. Traditional treatments, like chemotherapy, didn’t work well for them. But after genomic testing, doctors discovered a specific mutation in the BRAF gene. With this crucial information, they prescribed Dabrafenib, a BRAF inhibitor designed to target and block the mutated BRAF protein. This targeted therapy resulted in significant tumor shrinkage and a marked improvement in the patient’s overall survival. This example highlights just how transformative genomic testing can be in personalizing cancer treatment and improving outcomes.
Genomic testing is a pivotal component of personalized cancer treatment, providing essential insights into the genetic underpinnings of cancer. By identifying specific mutations and alterations in cancer cells, genomic testing enables the development of targeted therapies that can significantly enhance treatment efficacy and patient outcomes. As technology advances, the role of genomic testing in cancer care continues to grow, offering hope for more effective and individualized treatment options.
2. Biomarker Analysis
Biomarker analysis plays a crucial role in personalized cancer treatment by providing valuable information about the presence, progression, and characteristics of cancer. Biomarkers are biological molecules found in blood, other body fluids, or tissues that indicate normal or abnormal processes, including cancer. They help in diagnosing cancer, predicting its progression, and guiding treatment decisions.
Types of Biomarkers
1. Predictive Biomarkers
Predictive biomarkers give us clues about how likely a patient is to respond to a specific treatment. They help pinpoint which therapies are most likely to work based on the presence of certain biomarkers. For instance, the HER2 protein is a well-known predictive biomarker in cancer treatment. When HER2 is overexpressed, it’s often linked to aggressive breast cancer. Testing for HER2 in breast cancer patients helps decide if they’d benefit from HER2-targeted therapies like Trastuzumab (Herceptin). Patients with HER2-positive tumors usually see a better response to these treatments compared to those with HER2-negative tumors.
Prognostic biomarkers provide insights into the likely course or outcome of the disease, regardless of the treatment being used. They help predict the overall prognosis and survival chances of cancer patients. For example, the tumor marker CA-125 is used as a prognostic biomarker for ovarian cancer. Higher levels of CA-125 in the blood can indicate a higher risk of cancer recurrence and help track the disease’s progression. Monitoring CA-125 levels over time helps assess treatment effectiveness and guide further management decisions.
Diagnostic biomarkers are crucial for identifying the presence of cancer. They help detect cancer early, confirm a diagnosis, or distinguish between different cancer types. Prostate-specific antigen (PSA) is a common diagnostic biomarker for prostate cancer. Elevated PSA levels in the blood can suggest prostate cancer, though high PSA levels can also occur in non-cancerous conditions. PSA testing, along with other diagnostic methods, plays a key role in the early detection and diagnosis of prostate cancer.
Applications of Biomarker Analysis
a. Diagnosis and Early Detection: Biomarkers play a crucial role in catching cancer early, which is key for successful treatment. For instance, liquid biopsy tests can detect circulating tumor DNA (ctDNA) in blood samples. This non-invasive method helps spot cancer early and keeps track of its progression.
b. Personalized Treatment Plans: By analyzing biomarkers, doctors can customize treatment plans for each patient. For example, testing for specific mutations or protein expressions helps choose targeted therapies that are more likely to work for the patient's unique cancer type.
c. Monitoring and Managing Disease: Biomarkers are also useful for keeping an eye on how well treatments are working and managing disease progression. Regularly checking biomarkers like CA-125 for ovarian cancer or CEA (Carcinoembryonic Antigen) for colorectal cancer helps evaluate treatment response and spot any potential recurrences early on.
d. Predicting Treatment Response: Biomarkers can predict how well a patient might respond to a particular therapy. This helps in fine-tuning treatment plans and avoiding ineffective treatments. For example, testing for KRAS gene mutations can indicate whether patients with colorectal cancer are likely to benefit from EGFR inhibitors.
Case Study: Use of Biomarkers in Lung Cancer
Imagine a patient diagnosed with non-small cell lung cancer (NSCLC). Biomarker analysis reveals an EGFR mutation, which is important because these mutations are known to respond well to certain tyrosine kinase inhibitors (TKIs) like Erlotinib or Gefitinib. With this information, the oncologist prescribes one of these TKIs as part of the treatment plan. The patient ends up responding really well to the targeted therapy, seeing significant tumor shrinkage and improved survival. This example shows how biomarker analysis can steer treatment decisions and lead to better outcomes.
Biomarker analysis is crucial for personalized cancer care. It helps doctors choose the most suitable treatments and keep track of how well they’re working. By focusing on specific biomarkers, doctors can customize therapies for each patient, enhancing both effectiveness and results. As technology advances, biomarkers will continue to provide even more precise and personalized treatment options.
3. Targeted Therapies
Targeted therapies are cutting-edge approaches to cancer treatment that aim to specifically attack cancer cells while sparing normal cells. Unlike traditional chemotherapy, which destroys all rapidly dividing cells (both cancerous and healthy), targeted therapies zero in on specific molecules or pathways crucial for cancer cell growth and survival. This precision means that targeted therapies can be more effective and often come with fewer side effects.Types of Targeted Therapies
1. Monoclonal Antibodies:
These are lab-made molecules designed to target specific proteins on cancer cells. They work by either blocking the growth signals to cancer cells, bringing in immune cells to destroy them, or delivering toxic substances directly to the tumor. For example, Trastuzumab (Herceptin) is used for HER2-positive breast cancer. HER2 is a protein that helps cancer cells grow, and Trastuzumab targets and binds to HER2-positive cells. This binding stops HER2 from sending growth signals, slowing down or halting tumor growth and making other treatments like chemotherapy more effective.
2. Tyrosine Kinase Inhibitors (TKIs):
TKIs block the action of certain enzymes called tyrosine kinases, which are involved in cancer cell growth and survival. By inhibiting these enzymes, TKIs disrupt how cancer cells grow and spread. Imatinib (Gleevec) is a TKI used to treat chronic myeloid leukaemia (CML) and gastrointestinal stromal tumors (GISTs). It targets the BCR-ABL protein, a tyrosine kinase produced by a genetic mutation in CML cells, helping to control cancer cell proliferation.
3. Angiogenesis Inhibitors:
These drugs prevent tumors from forming new blood vessels, which they need to grow and spread. By cutting off this blood supply, angiogenesis inhibitors starve tumors of nutrients and oxygen, slowing or stopping their growth. For example, Bevacizumab (Avastin) is used for cancers like colorectal, lung, and kidney cancers. It targets and blocks vascular endothelial growth factor (VEGF), a protein that helps form new blood vessels. By inhibiting VEGF, Bevacizumab reduces the blood supply to the tumor, slowing its growth.
4. Hormone Therapies:
These are used for cancers that depend on hormones, such as breast and prostate cancers. Hormone therapies work by blocking the body’s natural hormones or interfering with hormone receptors on cancer cells. Tamoxifen, for instance, is used for estrogen receptor-positive breast cancer. It blocks estrogen from binding to its receptor on cancer cells, slowing or stopping the growth of tumors that need estrogen to grow.
5. PARP Inhibitors:
These drugs are used for cancers with BRCA1 or BRCA2 mutations. They block the repair of DNA damage in cancer cells, leading to cell death. Olaparib (Lynparza) is a PARP inhibitor used for treating ovarian cancer with BRCA mutations. By stopping the PARP enzyme from repairing DNA, Olaparib causes cancer cells to die and helps shrink tumors.
6. Checkpoint Inhibitors:
These are a type of immunotherapy that blocks proteins cancer cells use to avoid being attacked by the immune system. By inhibiting these “checkpoints,” these drugs help the immune system recognize and attack cancer cells more effectively. Pembrolizumab (Keytruda) and Nivolumab (Opdivo) are examples that target the PD-1/PD-L1 pathway, which cancer cells often use to hide from the immune system. Blocking this pathway boosts the immune system’s ability to fight cancer.
Advantages of Targeted Therapies
a. Increased Precision: Targeted therapies focus on specific molecular targets associated with cancer, leading to more precise treatment and reduced damage to normal cells.b. Reduced Side Effects: By targeting cancer-specific pathways, these therapies often result in fewer side effects compared to traditional treatments like chemotherapy.
c. Enhanced Efficacy: Targeted therapies can be highly effective in treating cancers with specific molecular alterations, leading to improved outcomes and prolonged survival.
Case Study: Targeted Therapy in Lung Cancer
Consider a patient diagnosed with advanced non-small cell lung cancer (NSCLC). Genomic testing reveals a mutation in the ALK gene (anaplastic lymphoma kinase). This genetic alteration is associated with a type of lung cancer that responds well to ALK inhibitors. The patient is prescribed Crizotinib (Xalkori), an ALK inhibitor. Crizotinib specifically targets and blocks the activity of the ALK protein, leading to significant tumor shrinkage and improved patient survival. This example illustrates how targeted therapies can provide effective treatment options based on specific genetic mutations.
Targeted therapies are a major leap forward in cancer treatment, offering a more precise approach compared to traditional methods. These therapies zero in on specific molecules crucial for cancer growth, resulting in better outcomes and fewer side effects. As research uncovers new targets, these therapies will continue to evolve, providing even more tailored options.
Immunotherapy is an exciting advancement in cancer treatment that uses the body's own immune system to combat cancer. Instead of directly attacking cancer cells like chemotherapy or radiation, immunotherapy boosts or restores the immune system’s ability to recognize and destroy cancer cells. This approach has made significant strides in treating various cancers and represents a major leap forward in personalized cancer care.
Types of Immunotherapy
1. Checkpoint Inhibitors:
These drugs block proteins that cancer cells use to hide from the immune system. By inhibiting these "checkpoints," the immune system can better detect and attack cancer cells. Pembrolizumab (Keytruda) and Nivolumab (Opdivo) are well-known examples. They target the PD-1/PD-L1 pathway, which cancer cells exploit to avoid immune detection. For instance, Pembrolizumab has shown impressive results in treating melanoma, lung cancer, and other cancers.
2. CAR-T Cell Therapy:
This innovative therapy involves modifying a patient’s T cells to recognize and attack cancer cells. T cells are collected from the patient, engineered to target specific cancer markers (like CD19), and then reintroduced into the body. Kymriah (tisagenlecleucel) and Yescarta (axicabtagene ciloleucel) are CAR-T therapies used for certain blood cancers like acute lymphoblastic leukemia (ALL) and large B-cell lymphoma. The engineered T cells then seek out and destroy cancer cells with the targeted antigen.
3. Monoclonal Antibodies:
These lab-created molecules target specific proteins on cancer or immune cells. They can directly kill cancer cells, block growth signals, or mark them for destruction by the immune system. Rituximab (Rituxan) is an example used to treat B-cell non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL). It targets the CD20 protein on B cells, marking them for immune destruction.
4. Cancer Vaccines:
Cancer vaccines help the immune system recognize and attack cancer cells by introducing cancer-specific antigens. There are therapeutic vaccines, which treat existing cancer, and prophylactic vaccines, which prevent cancer. Provenge (sipuleucel-T) is a therapeutic vaccine for prostate cancer made from a patient’s own dendritic cells. These cells are activated to target prostate cancer, prompting a strong immune response.
5. Oncolytic Virus Therapy:
This approach uses genetically modified viruses that specifically infect and kill cancer cells while leaving normal cells unharmed. These viruses can also stimulate the immune system to fight the cancer. Talimogene laherparepvec (T-VEC) is an example used for melanoma. It involves a modified herpes simplex virus that destroys melanoma cells and produces proteins that boost the immune response against the cancer.
Benefits of Immunotherapy
a. Enhanced Precision: Immunotherapy can be customized to target specific cancer markers or pathways, offering a highly personalized treatment option.
b. Durable Responses: Some patients experience long-lasting effects from immunotherapy, as it can help develop immune memory that continues to fight cancer even after treatment ends.
c. Potential for Broader Application: Immunotherapy holds promise for treating a wide range of cancers, including those that are tough to manage with traditional methods.
Case Study: Immunotherapy in Melanoma
A notable example of immunotherapy’s success is its use in treating melanoma. A patient with advanced melanoma was treated with Ipilimumab (Yervoy), a checkpoint inhibitor targeting CTLA-4, a protein that inhibits T cell activation. By blocking CTLA-4, Ipilimumab enhances T cell activity against cancer cells. This therapy led to a significant tumor regression and prolonged survival for the patient. Additionally, the patient experienced a durable response, demonstrating the long-term effectiveness of immunotherapy.
Immunotherapy transforms cancer treatment by harnessing the body’s immune system to attack cancer cells. With options like checkpoint inhibitors and CAR-T cell therapy, personalized treatments are advancing quickly. Ongoing research will likely enhance these therapies, offering new hope for more effective and personalized cancer care.
5. Personalized Drug Selection
Personalized drug selection involves choosing medications based on an individual patient's genetic, molecular, and clinical characteristics to optimize treatment efficacy and minimize side effects. This approach moves beyond the "one-size-fits-all" model, leveraging detailed information about a patient’s unique tumor profile and overall health to guide drug choices. By tailoring drug selection to the specific needs of each patient, personalized medicine aims to improve treatment outcomes and enhance patient quality of life.
Components of Personalized Drug Selection
Personalized drug selection tailors cancer therapies to the unique genetic, molecular, and personal characteristics of each patient. This approach enhances treatment efficacy and minimizes side effects. Here’s how it works:
1. Genetic and Molecular Profiling: This involves analyzing a patient’s tumor to identify specific genetic mutations, protein expressions, and other biomarkers. For example, in breast cancer, genomic profiling may reveal HER2 overexpression. In such cases, Trastuzumab (Herceptin), a monoclonal antibody targeting HER2-positive cells, may be prescribed to specifically address this alteration.
2. Pharmacogenomics: This field studies how genetic variations affect an individual's response to medications. For instance, Warfarin, an anticoagulant, is metabolized differently based on genetic variations in the CYP2C19 gene. Genetic testing can guide dosage adjustments to optimize effectiveness and minimize adverse effects, such as bleeding.
3. Tumor-Specific Drug Selection: Choosing treatments based on the unique characteristics of a patient’s tumor, such as genetic mutations, ensures targeted therapy. For example, Imatinib (Gleevec) is effective for Chronic Myeloid Leukemia (CML) patients with the BCR-ABL fusion gene, directly targeting the fusion protein involved in cancer cell proliferation.
4. Clinical Trials and Experimental Drugs: Personalized treatment may involve participating in clinical trials testing novel drugs or therapies. For example, patients with NTRK gene fusions might be eligible for trials of Larotrectinib (Vitrakvi), designed to target these specific genetic alterations.
5. Patient-Specific Factors: Effective treatment also considers individual patient factors such as overall health, coexisting conditions, and personal preferences. For example, a patient with kidney disease might need dose adjustments for drugs primarily excreted through the kidneys, ensuring the treatment plan is both safe and effective.
Benefits of Personalized Drug Selection
- Increased Efficacy: Drugs are chosen based on their specific action against identified tumor targets or genetic mutations, leading to more effective treatments.
- Reduced Side Effects: Tailoring drug selection based on genetic and molecular profiles helps avoid drugs that are likely to cause adverse reactions or have limited efficacy for the patient.
- Optimized Treatment Plans: Personalized drug selection allows for more precise dosing and scheduling, enhancing the overall effectiveness of the treatment plan.
Case Study: Personalized Drug Selection in Lung Cancer
A patient with advanced non-small cell lung cancer (NSCLC) undergoes genetic testing, which reveals a mutation in the EGFR gene. Based on this finding, the oncologist selects Erlotinib (Tarceva), a targeted therapy specifically designed to inhibit the mutated EGFR protein. This choice leads to a significant reduction in tumor size and improved progression-free survival for the patient. The personalized approach not only improves treatment outcomes but also minimizes the likelihood of unnecessary side effects associated with other treatments.
6. Advanced Imaging Techniques
Advanced imaging techniques are crucial in personalized cancer treatment as they provide detailed and precise visualizations of tumors, helping in accurate diagnosis, treatment planning, and monitoring. These technologies go beyond traditional imaging methods to offer enhanced resolution, functional insights, and molecular information, which are essential for tailoring individualized treatment strategies. Here’s a detailed look at some of the most advanced imaging techniques used in cancer care:
Types of Advanced Imaging Techniques
1. Positron Emission Tomography (PET) Scanning: PET scanning uses a radioactive tracer that emits positrons, which collide with electrons to produce gamma rays. These rays are detected to create images highlighting areas of high metabolic activity, often indicative of cancer. For example, 18F-FDG PET helps visualize cancer cells with high glucose metabolism, aiding in the detection and monitoring of lymphoma.
2. Computed Tomography (CT) Scanning with Contrast: CT scanning combines multiple X-ray images taken from various angles to create cross-sectional images of the body. When enhanced with contrast agents, CT scans provide detailed images of blood vessels and tissues, improving tumor visualization. CT angiography is useful for planning surgical interventions by visualizing the blood vessels supplying a tumor.
3. Magnetic Resonance Imaging (MRI): MRI employs strong magnetic fields and radio waves to produce high-resolution images of soft tissues. It is particularly effective for brain and spinal cord tumors. Functional MRI (fMRI) is used to map brain functions, which is crucial for planning surgeries involving brain tumors to avoid critical areas.
4. Molecular Imaging: This technique uses specific tracers to visualize molecular and cellular processes. Fluorescence Molecular Tomography (FMT) employs fluorescent probes to monitor tumor activity and distribution of targeted therapies, offering insights into tumor biology and treatment responses.
5. Diffuse Optical Imaging (DOI): DOI utilizes near-infrared light to evaluate tissue composition and detect abnormalities. It provides real-time information on tissue oxygenation and blood flow, which can help differentiate between benign and malignant breast lesions and assist in early diagnosis.
6. Photoacoustic Imaging: This method combines laser-induced ultrasound with optical imaging to assess tissue structure and function. It provides high-resolution images of tumor vascularity and oxygenation, useful for monitoring tumor blood flow and evaluating responses to anti-cancer therapies.
7. Hybrid Imaging Techniques: Hybrid imaging combines multiple modalities to offer a comprehensive diagnostic view. For instance, PET/CT integrates metabolic and anatomical information to precisely locate and characterize tumors, while PET/MRI combines high-resolution soft tissue imaging with metabolic data, enhancing evaluation and treatment planning.
Benefits of Advanced Imaging Techniques
a. Enhanced Precision: Advanced imaging provides highly detailed images that improve the accuracy of diagnosis, staging, and treatment planning.b. Real-Time Monitoring: Techniques like functional MRI and photoacoustic imaging allow for real-time monitoring of tumor response to treatment, facilitating timely adjustments to therapy.
d. Personalized Treatment: By offering insights into the specific characteristics of tumors and their microenvironment, advanced imaging helps in selecting the most effective and targeted treatments.
Case Study: Advanced Imaging in Prostate Cancer
A patient with prostate cancer undergoes multiparametric MRI (mpMRI), which combines T2-weighted imaging, diffusion-weighted imaging (DWI), and dynamic contrast-enhanced imaging (DCE). This comprehensive approach allows for precise localization and characterization of the tumor within the prostate. The imaging results help guide a targeted biopsy and the planning of a personalized treatment approach, which includes focal therapy to treat only the tumor while preserving surrounding healthy tissue.
7. Molecular Pathology
Molecular pathology is a specialized field that combines aspects of molecular biology and pathology to understand the molecular basis of diseases, particularly cancer. It involves analyzing genetic, epigenetic, and proteomic alterations in tissues to provide insights into disease mechanisms, diagnose conditions, and guide personalized treatment strategies. This approach enhances the precision of cancer care by identifying specific molecular changes that can be targeted by tailored therapies.
Key Components of Molecular Pathology
a. Genetic Analysis: Genetic analysis involves examining DNA sequences for mutations, amplifications, deletions, or other alterations linked to cancer. This method helps understand the genetic drivers of cancer and guides treatment choices. Next-Generation Sequencing (NGS) identifies genetic mutations in tumors. For instance, detecting BRCA1 or BRCA2 mutations in breast cancer can direct the use of PARP inhibitors like Olaparib, which target tumors with these specific mutations.
b. Gene Expression Profiling: Gene expression profiling assesses the activity of genes within a tumor to uncover patterns associated with various cancer types and prognoses. This information aids in diagnosing cancer, predicting disease progression, and selecting targeted therapies. Oncotype DX is a gene expression test used in breast cancer to evaluate the risk of recurrence and guide chemotherapy decisions. It analyzes the expression of multiple genes to predict the likelihood of cancer recurrence and the potential benefit of chemotherapy.
c. Proteomic Analysis: Proteomic analysis focuses on the study of proteins and their modifications in cancer cells. Since proteins are the functional products of genes, their expression and alterations provide insights into cancer biology and treatment strategies. Mass Spectrometry is used to identify proteins and their modifications in cancer tissues. For example, HER2 protein overexpression in breast cancer cells can lead to the use of HER2-targeted therapies such as Trastuzumab.
d. Epigenetic Analysis: Epigenetic analysis explores chemical changes to DNA and histones that affect gene expression without altering the DNA sequence. These modifications can impact cancer development and treatment response. DNA methylation profiling can identify abnormal methylation patterns in cancer. For instance, hypermethylation of the CDKN2A gene, which encodes a tumor suppressor protein, is often seen in various cancers and can be targeted by specific therapies.
e. Molecular Diagnostics: Molecular diagnostics use molecular techniques to detect specific biomarkers or genetic alterations associated with cancer. These tests are crucial for accurate diagnosis, prognosis, and treatment planning. FISH (Fluorescence In Situ Hybridization) detects genetic rearrangements and amplifications, such as the BCR-ABL fusion gene in chronic myeloid leukemia (CML). Identifying this fusion gene is essential for selecting tyrosine kinase inhibitors like Imatinib.
f. Tumor Microenvironment Analysis: Tumor microenvironment (TME) analysis investigates how surrounding stromal cells, extracellular matrix, and immune cells interact with cancer cells. This analysis reveals factors affecting tumor growth and response to treatment. Immunohistochemistry (IHC) studies the presence and distribution of immune cells and other TME components. Analyzing immune checkpoint proteins such as PD-L1 helps determine eligibility for immune checkpoint inhibitors like Pembrolizumab.
Benefits of Molecular Pathology
a. Enhanced Diagnosis: Molecular pathology provides detailed insights into the genetic and molecular alterations driving cancer, leading to more accurate diagnoses.b. Tailored Treatments: By identifying specific molecular targets, molecular pathology enables the use of targeted therapies that are more effective and have fewer side effects.
c. Prognostic Information: Molecular profiling helps in predicting disease progression and patient outcomes, allowing for more informed treatment decisions.
d. Personalized Care: Integrating molecular pathology into clinical practice ensures that treatment plans are customized to the unique molecular profile of each patient’s cancer.
Case Study: Molecular Pathology in Lung Cancer
A patient with non-small cell lung cancer (NSCLC) undergoes molecular pathology testing, including NGS and IHC, to analyze the tumor’s genetic and protein profiles. The tests reveal a EGFR mutation and high expression of PD-L1. Based on these findings, the oncologist prescribes Erlotinib, a targeted EGFR inhibitor, and considers Pembrolizumab, an immune checkpoint inhibitor, for additional treatment. This personalized approach improves treatment efficacy and helps manage the disease more effectively.
Molecular pathology is essential for personalized cancer treatment, offering deep insights into the genetic and molecular features of tumors. By using advanced techniques like gene profiling and molecular diagnostics, doctors can customize treatments to each patient's specific cancer characteristics, improving accuracy and outcomes.
Mediclinic City Hospital offers a range of personalized cancer treatments, supported by a team of experienced oncologists and genetic counselors. The hospital employs the latest in targeted therapies and immunotherapy, providing patients with cutting-edge cancer care.
- Established Year: 2008
- Location: 37 26th St - Umm Hurair 2 - Dubai Healthcare City, Dubai, United Arab Emirates
About The Hospital
- Mediclinic City Hospital is a state-of-the-art healthcare facility. It is equipped with the latest technology and staffed by highly trained professionals.
- Number of Beds: 280
- Number of Surgeons: 3
- The hospital boasts 80 doctors and over 30 specialists.
- Neonatal Beds: 27
- Operating Rooms: 6, plus 3 daycare surgery units, 1 C-section OT
- Cardiac Catheterisation Laboratories: 2
- Endoscopy suites, fully equipped laboratory, emergency department, labour and post-natal wards.
- Advanced Medical Technology: PET/CT, SPECT CT, and 3T MRI.
- The hospital offers specialist-focused treatment in areas such as cardiology, radiology, gynaecology, trauma, nuclear medicine, endocrinology, and more.
- Mediclinic City Hospital offers specialities in Urology, Neurology, Gynaecology, General Surgery, Gastroenterology, E.N.T, Dermatology, Cardiology, Oncology, Orthopedics, Ophthalmology, Bariatric Surgery, Paediatric Neurology, Paediatric Oncology, and Paediatric Orthopaedics, staffed by top doctors in each field.
Burjeel Medical City is equipped with state-of-the-art technology and a multidisciplinary team of oncologists, radiologists, and geneticists. The hospital offers comprehensive genomic testing and personalized treatment plans. The hospital has specialized programs for various cancers, including breast cancer, lung cancer, and colorectal cancer, utilizing targeted therapies and immunotherapy.
- Established Year: 2012
- Location: 28th St - Mohamed Bin Zayed City - Abu Dhabi - United Arab Emirates, United Arab Emirates
About The Hospital:
- Total Number of Beds: 180ICU Beds: 31 (Including 13 Neonatal ICU and 18 Adult ICU Beds)
- Labour and Delivery Suites: 8
- Operation Theatres: 10 (Including 1 state-of-the-art Hybrid OR)
- Day Care Beds: 42
- Dialysis Beds: 13
- Endoscopy Beds: 4
- IVF Beds: 5
- OR Day Care Beds: 20
- Emergency Beds: 22
- Individual Patient Rooms: 135
- 1.5 & 3.0 Tesla MRI and 64-slice CT scan
- Luxury Suites: Royal Suites: 6000 sq. ft. each
- Presidential Suites: 3000 sq. ft.
- Majestic Suites
- Executive Suites
- Premier & Deluxe Rooms
- Designed to be a hub for tertiary and quaternary oncology treatment.
- Specializes in adult and pediatric subspecialties, long-term, and palliative care.
- Offers immunotherapy and molecularly targeted therapies.
- Provides state-of-the-art diagnosis and compassionate treatment.
- Offers exceptional support services for patients and their families.
- Burjeel Medical City in Abu Dhabi offers advanced care and expertise in cardiology, paediatrics, ophthalmology, oncology, IVF, gynaecology & obstetrics, orthopaedics & sports medicine, a dedicated Shoulder and Upper Limb Unit, Burjeel Vascular Centre, and bariatric & metabolic surgery. This state-of-the-art hospital provides comprehensive, top-quality healthcare services to patients, ensuring their unique medical needs are met with the highest level of care and expertise. Burjeel Medical City is committed to providing high-quality medical care in a comfortable and technologically advanced environment.
- Address: 19th St - Oud Metha - Dubai - United Arab Emirates
- Number Of Beds: 252
- Number of ICU Beds: 43
About American Hospital:
- Premier private healthcare provider in the Middle East
- Part of Mohamed & Obaid Al Mulla Group
- Established to provide world-class medical service since 1996
- First hospital in the Middle East awarded JCI accreditation
- The comprehensive range of medical and surgical specialities across 40 disciplines
Accreditations and Awards:
- JCI accreditation
- Mayo Care Network member
- Ultrasound practice accreditation from AIUM
Specialities and Departments:
Several top hospitals in the UAE have adopted robotic-assisted radiation therapy, providing patients with access to some of the best cancer treatment options available worldwide.
Advantages of Personalized Cancer Treatment
a. Improved Efficacy: By targeting specific cancer mutations, treatments are more effective.b. Reduced Side Effects: Personalized treatments can minimize side effects compared to traditional chemotherapy and radiation.
c. Better Prognosis: Tailored therapies can lead to better survival rates and quality of life for patients.
How can HealthTrip assist with your treatment?
If you're seeking treatment, let HealthTrip be your compass. We support you throughout your medical journey with the following:
- Access to top doctors in 38+ countries and the largest health travel platform.
- Partnerships with 1500+ hospitals, including Fortis, Medanta, and more.
- Treatments in neuro, cardiac care, transplants, aesthetics, and wellness.
- Post-treatment care and assistance.
- Teleconsultations with leading doctors at $1/minute.
- Over 61K patients served.
- Access Top treatments and packages, such as Angiograms and many more.
- Gain insights from genuine patient experiences and testimonials.
- Stay updated with our medical blog.
- 24/7 unwavering support, from hospital formalities to travel arrangements or emergencies.
Hear from our satisfied patients
Personalized cancer treatment is revolutionizing the way cancer is treated, offering hope for better outcomes and improved quality of life for patients. By incorporating genomic testing, biomarker analysis, targeted therapies, immunotherapy, and other advanced techniques, personalized treatment plans provide a tailored approach that is more effective and less toxic than traditional methods. Leading hospitals in the UAE are at the forefront of this innovation, ensuring that patients receive the most advanced and individualized care possible.
Related Blogs
Urethral Cancer Treatment in the UK: Specialized Care for Patients from Russia
Urethral cancer, a rare and often challenging condition, requires specialized

Cervical Cancer Treatment in the UK: Comprehensive Care for Patients from Russia
Cervical cancer, a significant health concern for women worldwide, requires
Advances in Lymphoma Treatment in the UK
Navigating lymphoma treatment options can be overwhelming, especially for patients

Personalized Treatment Plans for Ovarian Cancer at Bumrungrad Hospital
Ovarian cancer is a complex and often challenging diagnosis, requiring

Targeted Therapy for Breast Cancer: Personalized Treatment Plans at Bumrungrad
Breast cancer is one of the most common cancers affecting

Innovative Breast Cancer Surgery at Bumrungrad
Breast cancer remains one of the most common cancers affecting