Pancreatic Cancer Treatment Options in the UK: A Guide for Patients from Russia
01 Aug, 2024
 Healthtrip Team
Healthtrip TeamFacing a diagnosis of pancreatic cancer can be overwhelming, especially when considering treatment abroad. For patients from Russia, the UK is known for its advanced medical care, cutting-edge technology, and expert oncologists. This guide aims to provide clear and accessible information about the treatment options available in the UK, helping you navigate this challenging journey with confidence.
Most popular procedures in India
Pancreatic Cancer
Pancreatic cancer occurs when malignant cells form in the pancreas, an organ behind the stomach that helps with digestion and blood sugar regulation. There are two main types of pancreatic cancer: exocrine tumors (the most common type) and endocrine tumors (less common but sometimes easier to treat).
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
Diagnostic Process
Early and accurate diagnosis is crucial for effective treatment of pancreatic cancer. In the UK, the diagnostic process involves several key steps to ensure a comprehensive understanding of the disease.
1. Imaging Tests
A. CT Scans (Computed Tomography)
A CT scan uses X-rays to capture multiple cross-sectional images of the body. These images are then combined into detailed 3D views of the pancreas and surrounding organs. This helps visualize the size, shape, and location of the tumor and assess whether it has spread to nearby structures. The procedure involves lying on a table that moves through a large, ring-shaped machine. You may need to fast for a few hours before the scan, and a contrast dye is often used to enhance the images.
B. MRI Scans (Magnetic Resonance Imaging)
MRI scans use magnetic fields and radio waves to produce high-resolution images of soft tissues. During the procedure, you lie on a table that slides into a cylindrical machine. MRI is particularly useful for examining the extent of the tumor and its involvement with nearby blood vessels. Preparation typically involves fasting for a few hours, and if a contrast agent is used, it will be injected to enhance the images.
C. PET Scans (Positron Emission Tomography)
A PET scan involves injecting a small amount of radioactive glucose into the bloodstream. Cancer cells absorb this glucose more readily, making them visible on the scan. The procedure requires lying on a table that moves through a PET scanner, which detects the radioactive signals and creates images of areas with increased glucose uptake. You will need to fast for several hours before the scan, and it’s advisable to avoid strenuous activities the day before.
2. Endoscopic Ultrasound (EUS)
Endoscopic Ultrasound (EUS) involves inserting an endoscope—a flexible tube with a camera and ultrasound probe—through the mouth and into the stomach and duodenum. The ultrasound probe emits sound waves that produce detailed images of the pancreas and surrounding tissues. EUS provides high-resolution images and is particularly useful for examining small tumors and assessing their relationship with nearby organs. The procedure also allows for guided biopsy, where a needle is used to collect tissue samples from the pancreas or nearby lymph nodes. You will need to fast for at least 6 hours before the procedure. Sedation is administered to help you remain comfortable, and it’s important to arrange for someone to drive you home afterwards.
C. Biopsy
A. Fine Needle Aspiration (FNA)
Fine Needle Aspiration (FNA) involves using a thin needle, guided by imaging techniques such as CT or EUS, to extract a small tissue sample from the pancreas. This sample is examined under a microscope to confirm the presence of cancer cells and to determine the type and grade of the tumor. The procedure is usually performed on an outpatient basis, and you may need to fast before it. Local anaesthesia is used to numb the area.
B. Endoscopic Biopsy
During an endoscopic biopsy, an endoscope is used to obtain tissue samples from the pancreas through the digestive tract. This method is used when the tumor is accessible via the digestive tract and provides critical information for diagnosis and treatment planning. You will need to fast before the procedure, and sedation will be given to ensure comfort. Arrange for transportation home afterwards.
4. Blood Tests
A. Tumor Markers
Blood tests for tumor markers such as CA 19-9 and CEA are used to monitor the progression of pancreatic cancer and the response to treatment. Elevated levels of these markers can indicate the presence of cancer or its progression, although they are not definitive on their own.
B. General Health Assessment
Blood tests also include liver and kidney function tests, which assess the health of these organs and ensure they are functioning properly before undergoing treatment. A Complete Blood Count (CBC) measures various blood components to detect anaemia, infection, and overall health status. These tests provide valuable information for planning and monitoring treatment. Together, these diagnostic tools and tests provide a comprehensive picture of the disease, guiding the development of an effective treatment plan and offering a clearer understanding of the cancer's progression.
Treatment Options
When it comes to treating pancreatic cancer, the approach depends on various factors, including the cancer's stage, location, and the patient's overall health. In the UK, a multidisciplinary team of specialists often collaborates to design a personalized treatment plan. Here’s a detailed look at the primary treatment options available:
1. Surgery
A. Whipple Procedure (Pancreaticoduodenectomy)
The Whipple procedure is a common surgical treatment for pancreatic cancer, particularly when the tumor is localized and operable. This complex surgery involves removing the head of the pancreas, the duodenum (first part of the small intestine), a portion of the stomach, the gallbladder, and sometimes part of the bile duct. The remaining pancreas, stomach, and intestines are then reconnected. This procedure aims to remove the cancerous tumor and affected tissues while preserving as much pancreatic function as possible. Recovery from the Whipple procedure can be extensive, often requiring a hospital stay of several weeks and a gradual return to normal activities.
B. Distal Pancreatectomy
A distal pancreatectomy involves the removal of the body and tail of the pancreas, along with the spleen. This procedure is generally considered when the tumor is located in the body or tail of the pancreas and has not spread extensively. Depending on the tumor's characteristics, additional nearby tissues or organs may also be removed. Post-surgery, patients may need to manage diabetes and enzyme replacement therapy, as a significant portion of the pancreas is removed.
C. Total Pancreatectomy
In cases where the cancer is widespread within the pancreas or involves nearby structures, a total pancreatectomy may be performed. This involves the removal of the entire pancreas, as well as the spleen, gallbladder, and portions of the stomach and intestines if necessary. This surgery significantly impacts digestion and blood sugar regulation, requiring lifelong management of insulin and pancreatic enzymes.
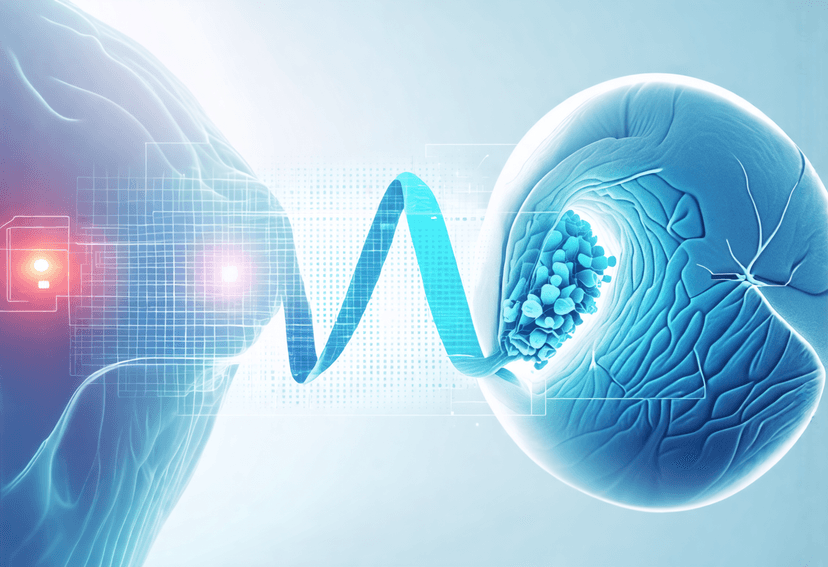
2. Radiation Therapy
A. External Beam Radiation Therapy
External beam radiation therapy directs high-energy rays from outside the body to the cancerous area. The treatment is typically given in daily sessions over several weeks. Radiation therapy is used to target and kill cancer cells, shrink tumors, and reduce symptoms, especially if the cancer is not resectable or if surgery is not an option. It can also be used in combination with chemotherapy to enhance treatment effectiveness.
B. Stereotactic Body Radiotherapy (SBRT)
SBRT is a more advanced form of radiation therapy that delivers high doses of radiation with pinpoint accuracy to the tumor. It is often used for patients with localized pancreatic cancer that is not amenable to surgery. SBRT typically requires fewer treatment sessions compared to traditional radiation therapy and is designed to minimize damage to surrounding healthy tissues.
3. Chemotherapy
A. Adjuvant Chemotherapy
Adjuvant chemotherapy is used after surgery to kill any remaining cancer cells that may not be visible or detectable. Common regimens include FOLFIRINOX (a combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin) and Gemcitabine-based therapies. The goal is to reduce the risk of cancer recurrence and improve survival rates.
B. Neoadjuvant Chemotherapy
Neoadjuvant chemotherapy is administered before surgery to shrink the tumor and make it more manageable for surgical removal. This approach can increase the likelihood of successful surgery and may also help in assessing the tumor’s response to treatment.
C. Palliative Chemotherapy
For advanced pancreatic cancer that cannot be surgically removed, palliative chemotherapy is used to manage symptoms, control tumor growth, and improve quality of life. Regimens may include Gemcitabine alone or in combination with other drugs like nab-paclitaxel or erlotinib. The focus is on prolonging life and alleviating symptoms rather than curing the disease.
4. Targeted Therapy
A. Targeted Drugs
Targeted therapy involves drugs that specifically target cancer cells' unique characteristics, such as genetic mutations or proteins that promote cancer growth. For pancreatic cancer, targeted therapies such as erlotinib (which inhibits the epidermal growth factor receptor, EGFR) are used in combination with chemotherapy for some patients. These therapies aim to block the growth and spread of cancer cells while minimizing damage to healthy cells.
B. PARP Inhibitors
For patients with certain genetic mutations, such as BRCA1 or BRCA2, PARP inhibitors may be used. These drugs block the repair of damaged DNA in cancer cells, leading to cell death. They are often used in cases where the cancer has spread beyond the pancreas.
5. Immunotherapy
A. Checkpoint Inhibitors
Immunotherapy is a newer treatment approach that uses the body’s immune system to fight cancer. Checkpoint inhibitors are drugs that help the immune system recognize and attack cancer cells more effectively. However, their use in pancreatic cancer is still under investigation and is typically considered for patients with specific genetic markers or clinical trials.
B. Vaccine Therapy
Experimental vaccine therapies are being explored as a way to stimulate the immune system to target pancreatic cancer cells. These vaccines are designed to provoke an immune response against cancer-specific antigens. Clinical trials are ongoing to evaluate their effectiveness.
6. Supportive Care and Palliative Care
A. Pain Management
Pain management is a critical aspect of pancreatic cancer treatment, particularly for patients with advanced disease. Pain relief may involve medications, nerve blocks, or other interventions to improve comfort and quality of life.
B. Nutritional Support
As pancreatic cancer can affect digestion and nutrient absorption, nutritional support is important. A dietitian may provide guidance on managing dietary changes, supplementing with pancreatic enzymes, and maintaining nutritional health.
C. Psychological and Emotional Support
Coping with cancer can be emotionally challenging. Support from counsellors, psychologists, or support groups can help patients and their families deal with the emotional aspects of the diagnosis and treatment.
In the UK, treatment plans are tailored to each patient's unique situation, and a multidisciplinary team of specialists ensures that all aspects of care are addressed comprehensively. This approach aims to provide the best possible outcomes while addressing both the physical and emotional needs of patients.
Choosing the right treatment for pancreatic cancer can be daunting, especially when navigating a foreign healthcare system. The UK offers a range of advanced treatment options, supported by expert oncologists and state-of-the-art facilities. Russian patients seeking pancreatic cancer treatment in the UK can be assured of receiving high-quality care tailored to their specific needs. It’s essential to consult with healthcare providers to discuss the most suitable treatment plan and make informed decisions about your health journey.
Related Blogs

The Role of Surgery in Pancreatic Cancer
Understand the importance of surgery in treating pancreatic cancer
Pancreatic Cancer Treatment Options
Get informed about the various treatment options for pancreatic cancer

Pancreatic Cancer Treatment Abroad
Explore affordable and quality pancreatic cancer treatment options abroad
Urinary Bladder Carcinoma Radiation Therapy and Palliative Care
Radiation therapy can provide palliative care for urinary bladder carcinoma
Radiation Therapy for Bladder Cancer in Elderly Patients
Radiation therapy is a suitable treatment option for elderly patients
Bladder Cancer Treatment with Radiation Therapy and Immunotherapy
Learn about the combination of radiation therapy and immunotherapy for










