Herniated Discs: Causes, Symptoms, and Diagnosis
07 Oct, 2023
 Healthtrip Team
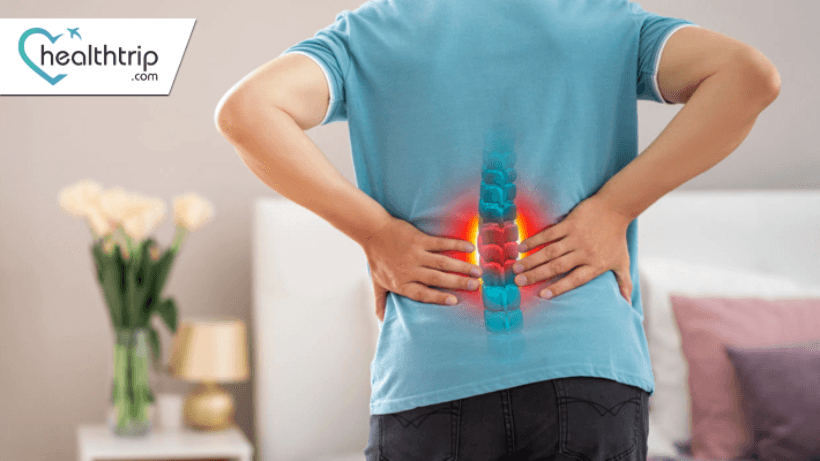
Healthtrip TeamImagine your spine as a stack of carefully arranged blocks, each representing a vertebra. Now, picture a soft, jelly-like cushion between these blocks – that's your intervertebral disc. These discs play a crucial role in providing flexibility and shock absorption to your spine. However, sometimes, life takes an unexpected turn, and these discs may herniate, causing discomfort and pain. In this blog, we will unravel the mystery behind herniated discs, exploring their causes, symptoms, and diagnosis.
Most popular procedures in India
Herniated Discs:
What Causes Herniation?
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
Herniated discs, also known as slipped or ruptured discs, occur when the soft inner portion of the disc protrudes through the tougher outer layer. Several factors contribute to this condition:
- Age-related Wear and Tear: As we age, our discs lose water content, making them less flexible and more prone to tearing.
- Improper Lifting Techniques: Lifting heavy objects using your back muscles instead of your legs can strain the spine and lead to disc herniation.
- Genetics: Some individuals may have a genetic predisposition to disc problems.
- Repetitive Strain: Activities that involve repetitive movements or heavy strain on the spine, such as sports or certain occupations, can increase the risk.
Identifying the Signs:
Symptoms of Herniated Discs:
Recognizing the symptoms is crucial for early intervention. Here are common signs of a herniated disc:
- Pain: The most prevalent symptom is localized or radiating pain, often felt in the buttocks, thighs, or calves.
- Numbness and Tingling: Herniated discs can compress nerves, leading to sensations of numbness and tingling in the affected area.
- Muscle Weakness: Weakness in specific muscle groups, usually in the legs, may be indicative of nerve compression.
- Changes in Reflexes: Reflexes may be diminished or exaggerated due to nerve compression.
Diagnosis of Herniated Discs
If you suspect a herniated disc, timely and accurate diagnosis is crucial for effective management. The diagnostic process is a meticulous journey that involves a combination of medical history exploration, physical examination, and advanced imaging techniques. Here's a more detailed breakdown of the diagnostic steps:
1. Medical History and Thorough Physical Examination:
The first step in diagnosing a herniated disc is a comprehensive review of your medical history. Your healthcare provider will delve into your symptoms, asking about the nature and duration of pain, any relevant medical conditions, and activities that may exacerbate or alleviate discomfort.
Following the discussion, a thorough physical examination is conducted. This examination aims to assess various aspects, including:
- Reflexes: Testing reflexes at specific points can provide insights into nerve function.
- Muscle Strength: Your healthcare provider may evaluate muscle strength in different areas of your body, especially in regions connected to the suspected herniation.
- Sensation: Assessing sensation involves checking for any numbness, tingling, or changes in sensitivity in specific regions of your body, which may indicate nerve involvement.
This combined history and physical examination provide valuable information that guides further diagnostic steps.
2. Imaging Tests: Unveiling the Inner Workings of the Spine
Advanced imaging plays a pivotal role in confirming the presence and determining the extent of a herniated disc. The most common imaging modalities include:
- X-rays: While X-rays don't directly show soft tissues like discs, they are useful in ruling out other conditions and providing a broad overview of the spine's structure.
- CT Scans (Computed Tomography): These scans offer detailed cross-sectional images of the spine, allowing for a closer look at the bones and the possibility of detecting herniated discs.
- MRI Scans (Magnetic Resonance Imaging): Considered the gold standard for diagnosing herniated discs, MRI scans provide high-resolution images of the soft tissues, including the intervertebral discs. This enables precise identification of herniations and their impact on nearby structures.
3. Electromyography (EMG): Decoding Electrical Signals in Muscles
When nerve compression and muscle damage are suspected, electromyography (EMG) becomes a valuable diagnostic tool. During an EMG, small needles are inserted into specific muscles, and electrical activity is measured. This helps identify abnormal electrical patterns, aiding in pinpointing the location and extent of nerve involvement.
EMG is particularly useful in distinguishing between nerve compression due to a herniated disc and other potential causes of muscle weakness or numbness.
4. Differential Diagnosis: Ruling Out Other Conditions
In certain cases, symptoms resembling a herniated disc may be caused by other spinal or neurological conditions. A thorough diagnostic approach involves ruling out alternative diagnoses through a process called differential diagnosis. This ensures that the chosen treatment plan is targeted and effective for the specific condition at hand.
Treatment Options for Herniated Discs
Dealing with a herniated disc can be challenging, but the journey to recovery involves various treatment options tailored to your specific condition. Here's a detailed exploration of the approaches to navigating the path to healing:
1. Rest and Activity Modification:
One of the primary recommendations for managing a herniated disc is allowing your body time to heal through rest. This doesn't mean complete immobilization, but rather a modification of activities that may exacerbate symptoms. Simple adjustments, such as avoiding prolonged sitting or lifting heavy objects, can significantly contribute to the healing process.
2. Physical Therapy:
Engaging in targeted exercises under the guidance of a physical therapist is a cornerstone of herniated disc treatment. These exercises aim to strengthen the muscles supporting the spine, improve flexibility, and alleviate pressure on the affected disc. Physical therapy sessions often include a combination of stretching, core stabilization, and aerobic exercises tailored to your individual needs.
3. Pain Medications:
Managing pain and inflammation is crucial for enhancing the quality of life during the recovery period. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen may be recommended. In more severe cases, prescription medications, such as muscle relaxants or stronger pain relievers, could be prescribed. It's crucial to use these medications under the supervision of a healthcare professional.
4. Epidural Steroid Injections:
For individuals experiencing persistent and severe pain, epidural steroid injections can provide targeted relief. These injections deliver corticosteroids directly into the epidural space around the spinal cord, reducing inflammation and providing temporary relief from pain. While not a long-term solution, they can be effective in managing symptoms, especially when combined with other therapies.
5. Chiropractic Care:
Chiropractic adjustments involve manual manipulation of the spine to alleviate pain and improve function. While not universally accepted as a primary treatment, some individuals find relief through chiropractic care. It's essential to consult with your healthcare provider before pursuing chiropractic treatment, especially in the context of a herniated disc.
6. Heat and Cold Therapy:
Applying heat or cold to the affected area can help manage pain and reduce inflammation. Heat therapy, through hot packs or warm baths, relaxes muscles and increases blood flow. Cold therapy, using ice packs, can numb the affected area, providing relief from pain and reducing swelling. Alternating between heat and cold may be recommended based on individual preferences and responses.
7. Lifestyle Modifications:
Beyond specific treatments, adopting a spine-friendly lifestyle is crucial for long-term well-being. This includes maintaining a healthy weight to reduce stress on the spine, practicing good posture in daily activities, and staying physically active to keep supporting muscles in optimal condition. These lifestyle adjustments contribute to overall spinal health and can prevent future occurrences of disc issues.
Diagnosing a herniated disc involves understanding patient symptoms, conducting a thorough physical exam, and utilizing advanced tools like MRI scans. This holistic approach empowers healthcare providers to craft personalized treatment plans for relief and recovery. If you suspect a herniated disc, prompt consultation with a healthcare professional is crucial for expert guidance.
Related Blogs
Complete Cost Breakdown of Eye Surgery with Healthtrip
Learn about doctors, hospitals, procedures, and recovery for eye surgery

How to Prepare for Your Eye Surgery in India
Learn about doctors, hospitals, procedures, and recovery for eye surgery
Side Effects and Risk Management of Eye Surgery
Learn about doctors, hospitals, procedures, and recovery for eye surgery

Follow-Up Care for Eye Surgery Patients with Healthtrip Assistance
Learn about doctors, hospitals, procedures, and recovery for eye surgery
Best Hospital Infrastructure for Eye Surgery
Learn about doctors, hospitals, procedures, and recovery for eye surgery
What to Expect During a Eye Surgery Consultation
Learn about doctors, hospitals, procedures, and recovery for eye surgery










